Performance Improvement
Accelerating Progress through Leadership Integration
Take four steps to break down operational silos
Your executive leadership team has been firing on all cylinders. Your CEO has emphasized the need for safety initiatives, undertaken high-reliability training, established safety huddles and connected real patient stories to your organization’s safety work. Your senior leaders have created an Office of Patient Experience and analyzed your data to prioritize improvement efforts. Your hospital or health system captures employee feedback every quarter and has your human resources leaders developing retention and resilience programs. Your organization’s quality teams have employed evidence-based practices and they are laser-focused on “meaningful measures.”
Trustee Talking Points
- Leadership teams may not always be convened around one aligned performance plan.
- Improvement initiatives and resources may therefore become uncoordinated and duplicative.
- Safety, quality, patient experience and workforce engagement are interdependent domains.
- Lack of a coordinated strategy for performance domains can undermine sustainable change.
So, with all of this progress, why does it feel like your senior leaders are climbing uphill every day?
The missing variable may rise well above these initiatives. While your organization’s efforts may individually address safety, quality, patient experience and workforce engagement, your leadership — and your resources — may not be convened around one aligned plan. Your organization may even be sacrificing the progress in one area when the spotlight is suddenly refocused on another low-performing department.
Both authors of this article have served on boards of health care organizations for more than a decade. Executives at our company visit hundreds of clients every year, and we repeatedly see lists of initiatives — department by department, floor by floor, unit by unit. Recently, we were at a large health system that, when audited, found more than 260 improvement initiatives. Every leader of these efforts had the best of intentions, but many were unaware of the volume, breadth and depth of the other initiatives. Without a strategy and action plan that aligns improvement efforts and acts on the interdependencies of safety, quality, patient experience and workforce engagement, siloed planning can undermine sustainable change.
What do we know about the relationships between the critical areas of operation? Based on integrated analyses of safety, quality, patient experience and workforce engagement data from millions of patient surveys, we can affirm the following:
- Health systems with better performance on “Likelihood to Recommend” and “Overall Rating” measures have net margins that are 4.8 and 3.0 percentage points higher, respectively, than those in the bottom quartile. Their median percentage of Medicare spending per episode of care allocated to within 30 days post-discharge was 2 percent and 2.3 percent lower, respectively, and their reimbursement per beneficiary was 2 percent and 4 percent lower, respectively.
- Health systems in the top quartile for “Likelihood to Recommend” and “Overall Hospital Rating” have, respectively, 4 percent and 13 percent lower rates of hospital-
acquired conditions, 15 percent and 23 percent shorter lengths of stay, and 3 percent each fewer readmissions than those in the bottom quartile. - Health systems in the top quartile for physician engagement have rates of hospital-acquired conditions that are 22 percent lower than those in the bottom quartile; and health systems in the top quartile for employee engagement have rates that are 6 percent lower than those in the bottom quartile.
- Health systems with highly engaged physicians have a median “Likelihood to Recommend” ranking that is 44 points higher than those with low levels of physician engagement.
These data validate the need for an integrated approach to leadership across the domains of safety, quality, patient experience and workforce engagement. Achieving such alignment requires vision and commitment. Following are four critical first steps toward leadership convergence under one unified strategy and related metrics.
Actively Encourage Leadership Convergence
In any sector, organizational operating models must be periodically evaluated and reorganized to maintain relevance to the market and enhance operating efficiency and effectiveness. Health care is no different, but health systems are often caught in the vicious cycle of thinking that what got us to where we are will get us to where we need to be. Nothing can be further from the truth. As the adage says, “Don’t let your past dictate your future.”
Our ability to challenge established norms and objectively evaluate how we are organized to perform will ensure that the needs of the organization are met. To fully realize the organizational benefits from the interconnectivity of safety, quality, patient experience and workforce engagement, organizations need to think differently about how they organize these leadership verticals.
There should be one strategy that connects all of these domains and one team to deliver on that strategy. For instance, the organizational strategy should focus on improving the patient experience, an approach that should include three elements — safety, quality and patient centeredness — as one concept. To execute on this approach, all functional areas responsible for operationalizing the three elements should have a common reporting structure.
Establish a Balanced Scorecard
Provider organizations have developed arrays of improvement initiatives, often in response to specific problems or regulatory mandates. These initiatives produce incremental improvement but are often uncoordinated and duplicative. Personnel working on them may be unaware of the efforts of their colleagues working on other initiatives.
This fragmented approach is increasingly being replaced by domain-specific efforts that are more effective in improving care for patients across the continuum of care. The leaders of these domains (safety, clinical quality, patient experience and workforce engagement) often know one another well, and when they work collaboratively toward the same goal, they can identify opportunities to integrate their efforts.
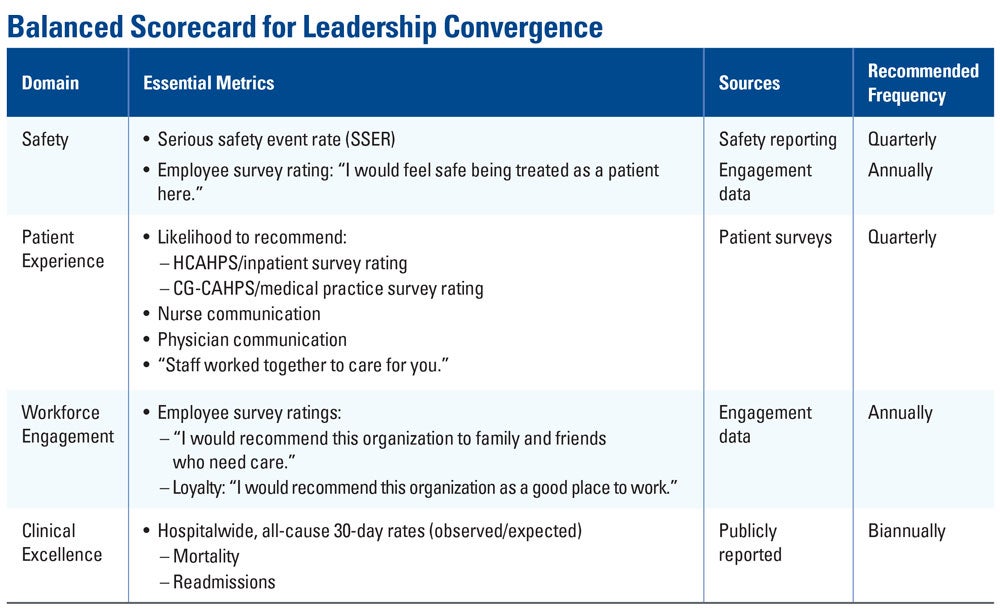
Based on our assessment of best practices, an integrated board scorecard should, in addition to financial performance, include performance on safety, patient experience, workforce engagement and clinical excellence.
By displaying essential metrics for the relevant domains in one place, scorecards allow leadership teams to regularly monitor progress in each domain over time and better understand and communicate the relationship between that progress and the overarching, unified goal of delivering optimally safe, effective, patient-centered care.
This balanced scorecard can display essential metrics in major domains, allowing boards and leaders to regularly monitor progress in each domain over time.
Support Your Executive Leadership Team
In order to facilitate true transformation, senior leaders must sometimes make difficult or unpopular decisions. If you believe in these individuals’ ability to successfully lead their teams, make sure they know you trust them with the mandate and have confidence in their decisions. Top CEOs know that they must nurture close relationships with their board to enable themselves to be nimble with decision making and garner support when needed.
Align Your Structure with Your Strategy
Meaningful structure facilitates alignment of day-to-day business with organizational strategy by establishing focus, holding stakeholders at all levels accountable and positioning them to succeed in a manner that is consistent with enterprise expectations.
To this end, organizations must be structured so that there is sufficient line of sight between the objectives of individuals, teams and the “big picture” — the health system’s vision. Every member of the organization should be clear on how the work in their area of responsibility connects to the work of others in different areas.
The board’s responsibility for good stewardship of the organization also requires guiding its culture, which requires championing a more strategic approach to people management. Health care human resources methodology has traditionally been very transactional, but this narrow approach can hinder progress in today’s challenging environment.
Trustee Takeaways
- Adopt a unified strategy and action plan to align improvement initiatives.
- Hold one team accountable for delivering on that strategy and action plan.
- Support senior leaders who must make difficult or unpopular decisions.
- Evaluate and reorganize operating models to ensure strategic relevance.
Instead, hospitals and health systems need to adopt a broader focus that encompasses not only whom they hire, but also how they on-board and prepare these people for their roles, how organizations develop them and how they are recognized and rewarded. In addition, it is incumbent on boards to ensure that organizations are tackling critical issues such as clinician burnout, workplace violence and bullying. This requires an organizational structure in which accountabilities are explicitly translated all the way to the job level.
Finally, the future of hospitals and systems is dependent on preparing the next generation of leadership through thoughtful succession planning. Recognizing the significant impact that extraordinary leaders have on organizational performance, preparedness for leadership turnover sets the stage for sustained leadership effectiveness, engagement and performance.
Conclusion
Health care delivery is challenging and highly nuanced. Health care leaders must consistently work to keep their strategies relevant and their organizations viable while striving to achieve high performance. Board members can help drive progress toward this goal by understanding the sector pressures and encouraging senior executives to break down the operational silos in order to execute on the interdependencies across the critical performance domains.
Patrick T. Ryan is CEO and James Merlino, M.D., is chief transformation officer at Press Ganey.